
General Practices in the UK now deliver a blend of in-person and remote consultations – by phone, online messaging and video. But as patients and practice teams adapt to this multi-modal system, questions remain: Who gets what kind of care? Why? And how do patients navigate a service that can often feel confusing, inconsistent and relationally remote?
We collaborated with Professor Sara Shaw and Natassia Brenman from the University of Oxford’s Nuffield Department of Primary Care Health Sciences, Sophie Spitters from the Centre for Primary Care at Queen Mary University of London, and the University of Manchester on an 18-month research project to explore these questions.

”We are excited to have this great resource to help our patients feel empowered to use our services, without feeling that there is a big barrier in the way.
”Sometimes we forget that patients don’t understand NHS systems and useful, simple and clear advice can really change attitudes and help people feel confident to manage their own health journeys.”
We supported both the research and design process, helping to develop practical tools for understanding and improving primary care experiences. Our contributions included:
Early prototypes took the form of posters and provocations that explored different types of language and openness, for example, expressing a practice’s aspirations for patient-centred care alongside its ongoing challenges with resources and community needs.

We ran online sessions and in-person workshops with practice staff and patient groups to gather lived experiences and test new ideas. We also worked closely with the research team to review and distil this feedback into a final set of co-designed journey cards for stakeholders to evaluate.


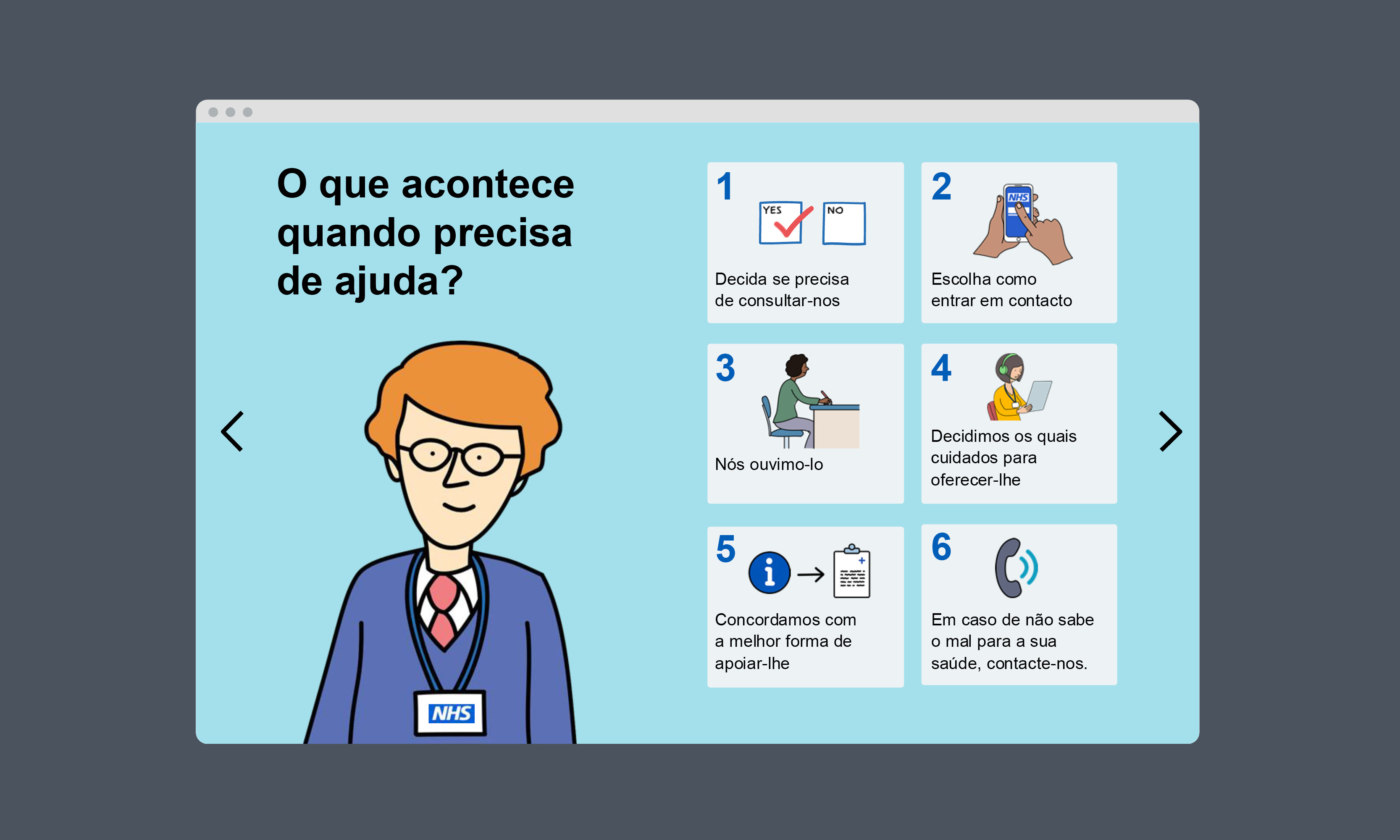
Following extensive co-design workshops, the researchers identified a critical gap: patients often struggled to understand the full journey from feeling unwell to receiving care. To help bridge this gap, we created a customisable template document for practices, tailored to their specific processes and communities.
The patient journey was structured around six key steps:
This resource offers practices a way to make the consultation process more transparent, accessible and patient-centred.

We translated the resource into Arabic and Portuguese to broaden accessibility. We plan to translate it into 10–15 additional languages after the initial pilot phase.

”Big Thanks to the ModCons team for helping us with this!”
This work is about more than documentation. It’s about equipping patients, providers and policymakers with tools to better navigate – and even shape – the future of primary care. It’s also part of wider research exploring the concept of ‘remote by default’, for which we have been helping the team develop a range of visually led policy notes. You can read about these here.
If you’re working in health or social care and want to turn complex systems into clear, people-centred communication, we’d love to hear from you.